Arthroscopic assessment of meniscal injuries using an anatomical zone classification system
Diego Costa Astur, Bruno Silveira Pavei, Pedro Barreira Cabral, Eduardo Vasconcelos Freitas, Camila Cohen Kaleka, Pedro Debieux, Daniel Esperante, Moises Cohen
Instituto Cohen, São Paulo, Brasil
RESUMEN
El propósito del presente estudio es evaluar la reproducibilidad inter e intraobservador de la clasificación artroscópica de lesiones meniscales propuesta por Śmigielski en pacientes tratados con suturas meniscales, así como correlacionar las zonas anatómicas con las características lesionales y el tipo de técnica de sutura empleada.
Se analizaron cuarenta y seis artroscopías de rodilla con sutura meniscal de la lesión. Se examinó la zona descripta según Śmigielski , el tipo de lesión meniscal, la vascularidad, la técnica de sutura meniscal y el tipo de nudo empleados. Los datos fueron evaluados para considerar la reproducibilidad intra e interobservador. Todos los resultados clínicos, anatómicos, características de la lesión, así como el tratamiento meniscal utilizado, se correlacionaron.
La correlación intra e interobservador (coeficiente Kappa) para la clasificación artroscópica de lesiones meniscales propuesta por Śmigielski fue leve o moderada. La clasificación por zonas que define la lesión meniscal y su relación con las estructuras anatómicas de la rodilla tiene aplicación limitada en la cirugía artroscópica. El conocimiento practico de la clasificación podría servir como guía para la toma de conducta ante las lesiones meniscales reparables.
ABSTRACT
The present study aimed to evaluate the inter- and intra-observer reproducibility of the arthroscopic meniscus tear classification system in patients treated with meniscal suture, as well as to correlate these anatomical zones, according to the injury characteristics and the suture technique employed.
Forty-six knee arthroscopies were analyzed for meniscal sutures. The evaluators recorded data of the zones described by Śmigielski, types of injuries, meniscal vascularity, suture techniques, and types of suture knots applied to sutures. Data were analyzed with respect to inter and intra-observer agreement. All clinical and anatomical outcomes as well as the characterization of the injury and meniscal treatment were correlated.
The intra- and inter-observer reproducibility (Kappa coefficient) for the arthroscopic classification system of meniscus injury proposed by Śmigielski ranged from slight to moderate.
The zone classification defines the menisci and their relationship with the surrounding anatomic landmarks of the knee; however, it has limited arthroscopic application. The practical knowledge of the classification system described in this study can help specifically guide treatment for various types of meniscal injury.
Keywords: Meniscal Injury; Meniscal Repair; Meniscal Suture; Anatomical Classification
INTRODUCTION
The meniscus is made of fibrocartilaginous tissue that protects and stabilizes the knee joint.1, 2 Meniscal tears can affect the normal distribution of load on the knee and may lead to degenerative joint changes, such as articular cartilage degeneration and symptomatic osteoarthritis.3 Surgical repair with sutures both preserves the meniscus structure and ensures the long-term survival of the knee joint.4, 5
The ideal suture technique for the meniscus depends on the location of the lesion, as well as anatomical and vascular characteristics.6 Accurate classification of the tear pattern, which is often done according to location based on blood supply (red-red zone, red-white zone and white-white zone), direction and type of meniscal injury (flap, radial tear, horizontal, longitudinal oblique or complex and degenerative) can guide the clinician in surgical planning.7-9
Even with the current prevailing trends in repairing meniscus-related lesions, healing rate after meniscal repair is 60%, and 3 to 32% of repairs fail, causing painful symptoms and functional impairment.10 The anatomical classification proposed by Śmigielski et al. distinguishes the medial and lateral menisci in anatomical zones according to their adjacent structures. Implementation of this classification system is also thought to increase understanding of meniscal injuries and can assist surgeons in selecting the most appropriate treatment.11
The present study aimed to evaluate the inter- and intra-observer reproducibility of the arthroscopic meniscus tear classification system in patients treated with meniscal suture, as well as to correlate these anatomical zones, according to the injury characteristics and the suture technique employed. The hypothesis of this study is that the anatomical classification can repeatably identify the main characteristics of meniscal injuries and suture technique according to their anatomical zone.
METHODS
A total of 440 patients diagnosed with meniscal injury and treated surgically between 2012 and 2017 were evaluated. Patients with meniscus tears repaired with techniques that included combined or solely inside-out, outside-in, and all-inside techniques, as well as meniscal reinsertion, were included in the study. While reviewing the arthroscopic findings, we excluded patients whose injuries could not be identified or comprehensively characterized. In total, forty-six patients were included in the study. Patient charts and arthroscopic recordings were analyzed and evaluated by three board-certified orthopedic surgeons with more than ten years of experience in treating meniscal injuries. There was no contact between these professionals throughout the study protocol and each surgeon completed the analysis twice, with a 3-month interval between evaluations. Surgeons received the videos in a random sequence and were not familiar with patients prior to analysis.
Data on demographics, time period from injury to surgery, and presence or absence of anterior cruciate ligament (ACL) with meniscus injury were recorded. The evaluating surgeons recorded the location of the lesions by meniscus zone according to the Śmigielski classification. Śmigielski et al. proposed an anatomical division of medial meniscus into five uneven anatomical zones: zone 1 (of the anterior root), zones 2a and b (anterolateral zone), zone 3 (the tibial collateral ligament- medial zone), zone 4 (the posterior zone) and the zone 5 (the posterior root). The lateral meniscus is divided into six anatomical zones: zone 1 (of the anterior root), zones 2a and b (anteromedial zone), zone 3 (popliteal hiatus zone), zones 4 and 5 (the posterior zone) and the zone 6 (of the posterior root)11, 12 (fig. 1).
The evaluators also recorded data on the zone of injury described by Śmigielski11, 12 that included meniscal tears classified according to their orientation (vertical longitudinal, vertical radial, horizontal, oblique or complex/degenerative), meniscal vascularization zone, repair techniques (all-inside, outside-in and inside-out, reinsertion of meniscal root) and suture configuration (horizontal, vertical, or cross stitch).7-9, 13
The collected data were analyzed by the Kappa statistic, frequently used to test inter- and intra-rater reliability. All outcomes corresponding to clinical and anatomical characterization of the lesion and meniscal treatment were correlated with each other.
The study was approved by the research Ethics Committee of the Universidade Federal de São Paulo – UNIFESP (case N. CAAE 75000717.9.0000.5505 and CEP 1084/2017).
Statistical analysis
An arbitrary division of results was used to determine the kappa values: A Kappa value below 0.0 suggests poor agreement, a Kappa value of 0.00 to 0.20 constitutes slight agreement, 0.20 to 0.40 is fair agreement, 0.41 to 0.60 is moderate agreement, 0.61 to 0.80 is substantial agreement, and 0.81 to 1.00 is almost perfect agreement. We used the test for equality of two ratios to compare whether the proportion of responses of two variables and/or their levels were statistically significant. The Chi-square test was used to determine if there was a significant relationship between two nominal (categorical) variables. The level of significance was set at 0.05 (5%), with a 95% confidence interval.
RESULTS
The total number of patients (n = 46) represented 10.4% of meniscal injuries treated. Of these, thirty-four patients had medial meniscus injury, and twelve lateral exhibited meniscus injury. The mean age of participants was 31.9 years (SD +/-3.2 years). The period between the diagnosis and the surgical procedure was 3.1 months (SD +/- 1.5 months; range: 0.1-24 months). Male patients (73%) were more prevalent (p<0.001). In addition, 46.7% of patients had a concomitant ACL injury. Soccer players were the most common group to suffer meniscal injury (36.8%) (p=0.02).
Meniscal zone
For the MM, 2% of the cases occurred in zone 2a, 18% in zone 2b, 38% in zone 3, 39% in zone 4, and 2% in zone 5 (p=0.206). For the LM, 5% of the cases occurred in zone 2a, 13% in zone 2b, 38% in zone 3, 39% in zone 4, and 3% in zone 5 (p=0.154) (fig. 1).
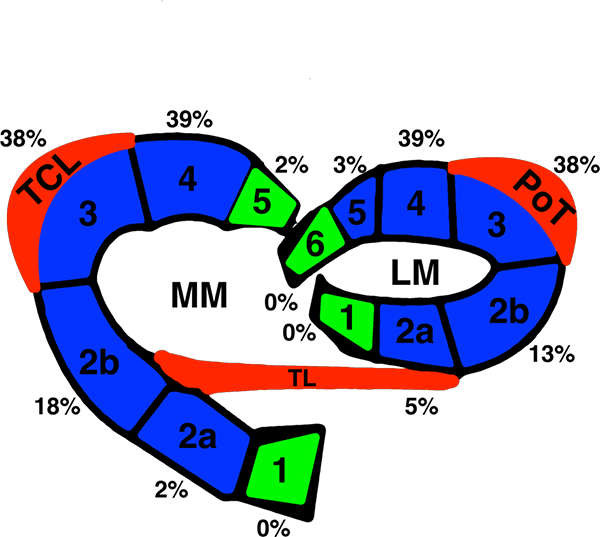
Figure 1: Schematic image showing the medial meniscus (MM) and lateral meniscus (ML) zones. Regarding the MM, zone 3 attaches to the tibia collateral ligament (TCL). In regard to the LM, the transverse ligament (TL) delineates zone 2 into two sub-zones: 2a and 2b; zone 3 attaches to the popliteal tendon (PoT). The percentages represent the meniscal injuries described in the present study.
Types of injuries
Regarding the MM injury patterns, 82% of the injuries were vertical longitudinal, 3% complex, 6% radial, 1% of the meniscal root, 6% meniscal flap, and 2% were horizontal longitudinal (p<0.001). For the LM, 62% of the injuries were vertical longitudinal, 14% complex, 12% radial, 4% of the meniscal root, 1% meniscal flap and 7% were horizontal longitudinal (p<0.001).
Intra-observer correlation
The Kappa coefficient obtained for the medial meniscus analysis was 0.586 (moderate) for observer A, 0.448 (moderate) for observer B, and 0.588 (moderate) for observer C. The Kappa coefficient obtained for the lateral meniscus analysis was 0.696 (substantial) for observer A, 0.528 (moderate) for observer B and 0.646 (moderate) for observer C. (Table 1).
Inter-observer correlation
The Kappa was calculated for two pairs of observers: for the medial meniscus, the agreement level for observers A and B was 0.399 (fair), between observers B and C 0.476 (moderate), between observers A and C 0.501 (moderate). For the lateral meniscus, the agreement level for observers A and B was 0.117 (slight), between B and C 0.386 (fair), and between A and C 0.265 (fair). (Table 1)
TABLE 1. KAPPA VALUES FOR INTER- AND INTRA-OBSERVER AGREEMENT IN THE ASSESSMENT OF MM AND LM
EXAMINERS |
|
A |
B |
C |
Intra-observer Kappa |
MM |
0.586 |
0.448 |
0.588 |
LM |
0.696 |
0.528 |
0.646 |
|
|
A/B |
B/C |
A/C |
Inter-observer Kappa |
MM |
0.399 |
0.476 |
0.501 |
LM |
0.117 |
0.386 |
0.265 |
Anatomic zone x vascular zone
For the MM, 48% of the injuries occurred in the red-white zone and among these, 42% occurred in zone 4. Among white-white zone injuries, 44% occurred in zone 4 and among red-red zone injuries 42% occurred in zone 3 (p<0.001). For the LM, 50% of the injuries occurred in red-white zone and among these, 35% occurred in zone 4 (p<0.001). The white-white zone injuries were most prevalent in zone 3 (30%) (p=0.002). The red-red zone injuries were most prevalent in zone 4 (38%) (p<0.001) (Table 2).
Type of injury by menical zone
Most MM injuries were longitudinal (82%) and occurred primarily in zones 3 (42%) and 4 (42%). Radial tears were predominant in zone 4 (40%). Horizontal tears were predominant in zones 3 (50%) and 4 (50%). Disinsertion of the meniscal root was the most common injury in zone 5 (90%) (p<0.001). Most LM injuries were longitudinal (61%) and occurred primarily in zone 4 (39%). Radial tears were predominant in zones 4, 5 and 6 (25%), while horizontal tears occurred predominantly in zone 2b (42%). All disinsertions of the meniscal root occurred in zone 6 (p<0.001) (Table 2).
TABLE 2. ABSOLUTE DATA FOR THE NUMBER OF CASES THAT INCLUDED VASCULAR ZONE, SUTURE TECHNIQUE, TYPE OF SUTURE KNOT, AND TYPE OF MENISCUS INJURY IN MM AND LM DIVIDED BY ZONES.
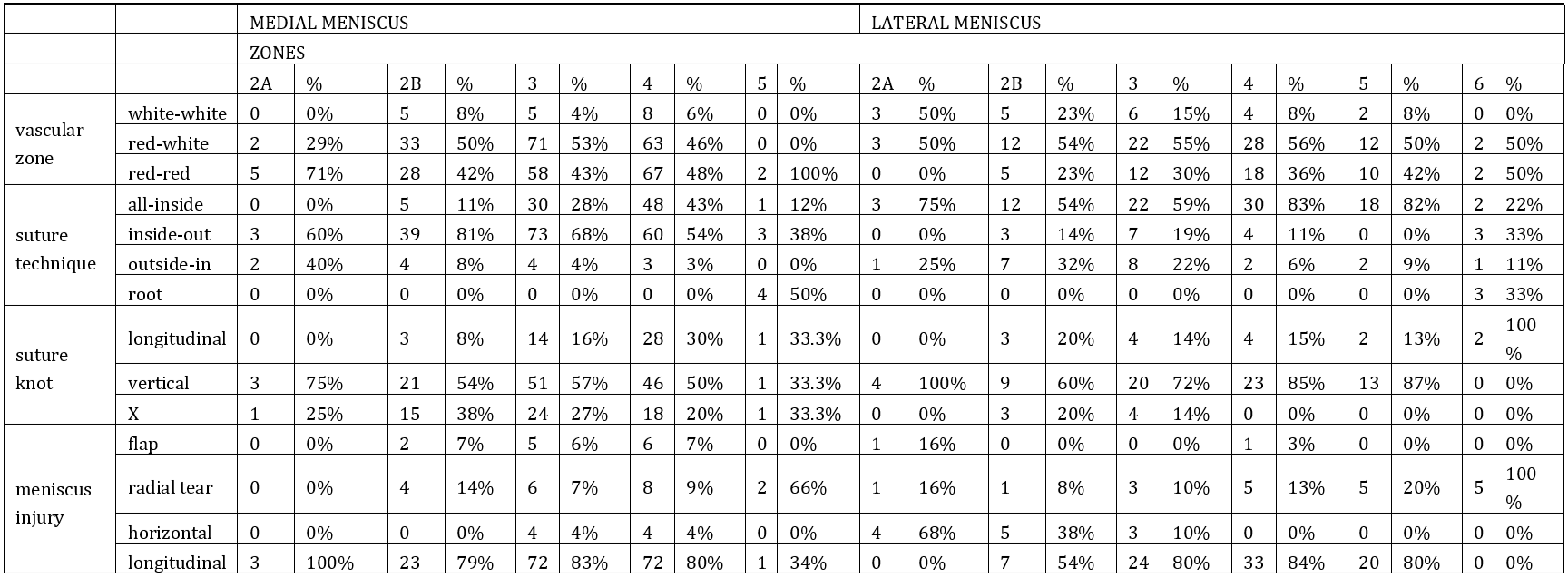
Suture technique by anatomic zones
The inside-out suture technique was used to repair the MM in 61% of the cases. The all-inside suture technique was commonly utilized to treat lesions in zone 4 (57%), and the inside-out suture technique used for lesions in zone 3 (41%). The outside-in suture technique was performed predominantly in zones 2b and 3 (31%) (p<0.001). In the LM, the all-inside suture technique was performed in 66% of the cases and predominantly in zone 4 (34%). The inside-out (41%) and the outside-in (33%) techniques were used in 3-zone meniscal injuries (p<0.001) (Table 2).
Type of suture by anatomic zone
For the MM, the vertical suture knot was used in 51% of the cases, predominantly in zone 3 (42%). The cross suture was held mainly in zone 3 (41%) (p<0.001). For the LM, the vertical suture knot was also the most used overall (72%), and in zone 4. The cross suture knot was predominantly used in zone 3 (57%) (p<0.001) (Table 2).
DISCUSSION
The present study evaluated the intra and inter-observer repeatability of the Śmigielski classification method when characterizing meniscal injuries. Although this classification method is clear and objective, when used to evaluate an arthroscopic repair, the intra-observer reproducibility was in the moderate to substantial range and the inter-observer reproducibility was in the slight to moderate range.
The intra-observer agreement for LM lesions was better than the intra-observer agreement obtained when classifying MM lesions, however, most values for Kappa statistics were considered moderate. The results of the inter-observer assessment for the medial meniscus were higher compared to those for the lateral meniscus. The values for Kappa statistics ranged from slight agreement to fair agreement.
The arthroscope allows an optimal visualization of the compartments of the knee, however, the meniscus anatomical and adjacent structures are not easily viewed through the arthroscope. The authors hypothesize this is the reason for the poor repeatability when the Śmigielski classification is used during arthroscopic surgery. Considering that this classification could impact the choice of meniscal suture techniques and patient care, it is imperative to ensure that this method is reliable intraoperatively or before surgery. Also, the type of suture used can interfere with resistance fixation. Vertical and cross sutures are stronger than the horizontal ones, whereas oblique sutures provide greater resistance fixation.14, 15 The meniscus and its associated structures anatomical characteristics in different zones make it more or less amenable to a given technique, suture configuration. Therefore, it is crucial to define the zones with lower suture failure rates, or with greater stability imparted by a given technique based on the injury zone. Herein lies the potential planning benefit of a classification system such as the one described by Śmigielski.
The extreme classification zones (zones 1 and 5 medial meniscus, zone 6 lateral meniscus) are the meniscal roots.16, 17 Although injuries in these zones are less common and have a low incidence when compared to the injuries of the other zones, all cases of injuries in these zones were treated with the meniscal root reinsertion, which is the current recommendation in the literature.18, 19
Zone 2 comprises the anteromedial portion of the meniscus. In the MM, this zone extends from the root zone to the medial collateral ligament (MCL). In the LM, it extends from the anterior root to the popliteal hiatus. The transverse ligament (TL) separates the meniscal zones into two sub-zones: 2a and 2b. In this zone, the meniscus is not attached to the joint capsule, but only to the tibia by the coronary ligaments.11, 12 Due to the anterior position of zone 2, the outside-in suture technique is more commonly used, corresponding to 40% and 46% for repairs of the LM and MM, respectively.
In the MM, zone 3 corresponds to the area covered by the MCL, where the MM is attached to the joint capsule, to the tibia by the coronary ligament, and to the femur by the menisco-femoral ligament (MFL).17 In the LM, zone 3 is the area covered by the popliteus hiatus where there is no meniscus-capsule attachment. Here, the meniscus is attached to the upper and lower popliteal meniscal ligament (PML) and to the menisco-fibular ligament (MFiL).20 This area is highly susceptible to MM and LM injuries (38%). This is the zone where the cross suture was the most frequently used (41% in MM and 56% in LM), possibly to the arthroscopic viewing angle and easier access compared to more complex sutures.21
In MM, zone 4 extends from the MCL to the posterior root. In this zone, the meniscus is not attached to the joint capsule, but only to the tibia by the coronary ligaments. In LM, zone 4 and 5 are attached to the joint capsule to the tibia by the coronary ligaments. Zone 5 is attached to the femur by the MFL. In our study, 39% of MM and LM injuries occurred in this zone. The prevalence of the all-inside technique in this zone (57% and 34% for medial and lateral menisci, respectively) may be due to the close proximity to neurovascular structures present between meniscus and skin, discouraging the use of the inside-out technique.14, 22 In LM, zone 5, which exhibits similar technical difficulties and neurovascular structures to zone 4, accounted for 21% of the injuries. Therefore, both LM zones (4 and 5) showed a significant number of injuries.
While the Śmigielski classification system does a great job describing the anatomy and theoretical suture choice to be used, it falls short in its implementation clinically, therefore a better arthroscopic classification system should be developed to better serve surgeons in the operating room. However, the Śmigielski classification does provide improved understanding about meniscal anatomy and helps to elucidate the reason for the occurrence of the meniscal tear and meniscal suture failure. Correlating injuries characteristics, locations and techniques may help surgeons to learn why different types of injuries happen, and failure rates remain high.
Even without optimal intra-operative, it could still be useful pre-operatively to plan the surgical procedure. For example, it could be used to evaluate an MRI, which removes the limitation of intra-operative visualization of meniscal anatomy and adjacent structures and define the correct zone of the meniscal injury to help plan the procedure. Implementation of this system could reduce the incidence of repair failures, providing function for the patient and improved prognosis of the affected knee joint.
The main limitation for this study is the small number of participants. Although the study size is large enough to result in statistical significance, implementing this classification technique on more patients will. Another limitation is that the classification system was applied retrospectively on videos of arthroscopic surgeries. Thus, the reliability of the technique may have been different when used during a live surgery, where views of the anatomy could be optimized. Future studies could look at the implementation of this technique on MRI or other imaging modalities that can better visualize anatomy.
CONCLUSION
The intra- and inter-observer reproducibility (Kappa coefficient) of the anatomical classification of menisci proposed by Śmigielski during arthroscopic ranged from slight to moderate agreement. In addition, most of the injuries were in the red zone (zone 4), longitudinal (zone 3 and 4). The most widely used suture technique was the inside-out for the MM and all-inside for the LM. Cross stich and vertical suture knots were mostly used in zones 3 and 4.
CONFLICTS OF INTEREST
The authors declare that there is no conflict of interest.
REFERENCES
- Barber BR; McNally EG. Meniscal injuries and imaging the postoperative meniscus. Radiol Clin North Am, 2013; 51(3): 371–91.
- Wadhwa V; Omar H; Coyner K; Khazzam M; Robertson W; Chhabra A. ISAKOS classification of meniscal tears—illustration on 2D and 3D isotropic spin echo MR imaging. Eur J Radiol, 2016; 85(1): 15–24.
- Siemieniuk RAC; Harris IA; Agoritsas T; Poolman RW; Brignardello-Petersen R; Van de Velde S; et al. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. BMJ, 2017; 357: j1982.
- Beaufils P; Pujol N. Management of traumatic meniscal tear and degenerative meniscal lesions. Save the meniscus. Orthop Traumatol Surg Res, 2017 103(8S): S237-S244.
- Perkins B; Gronbeck KR; Yue RA; Tompkins MA. Similar failure rate in immediate post-operative weight bearing versus protected weight bearing following meniscal repair on peripheral, vertical meniscal tears. Knee Surg Sport Traumatol Arthrosc, 2018; 26(8): 2245-50. DOI: 10.1007/s00167-017-4665-9
- Gomes AF; Paganella VC; Zapparoli M; Zanoni EK; Lucaski FF; Aguiar R. Rotura em “alça de balde” simultânea dos meniscos no mesmo joelho. Acta Ortop Bras, 2009; 17(4): 247–9.
- Arnoczky SP; Warren RF. Microvasculature of the human meniscus. Am J Sports Med, 1982; 10(2): 90–5.
- Arnoczky SP; Warren RF (1983) The microvasculature of the meniscus and its response to injury. Am J Sports Med, 1983; 11(3): 131–41.
- Cooper DE; Arnoczky SP; Warren RF. (1991) Meniscal repair. Clin Sports Med, 1991; 10(3): 529–48.
- Pujol N; Tardy N; Boisrenoult P; Beaufils P. Long-term outcomes of all-inside meniscal repair. Knee Surg Sports Traumatol Arthrosc, 2015; 23(1): 219–24.
- Śmigielski R; Becker R; Zdanowicz U; Ciszek B. Medial meniscus anatomy from basic science to treatment. Knee Surg Sports Traumatol Arthrosc, 2015; 23(1): 8–14.
- Śmigielski R. Anatomy of the meniscus - Paper presented at the 3rd International Meeting The meniscus preserve the future, Porto, Portugal 4-6 February 2016.
- Anderson AF; Irrgang JJ; Dunn W; Beaufils P; Cohen M; Cole BJ; et al. Interobserver Reliability of the International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine (ISAKOS) Classification of Meniscal Tears. Am J Sports Med, 2011; 39(5): 926–32.
- Astur DC; Pavei BS; Kaleka CC; Cohen M. Multiple hybrid sutures of bucket handle injury on the lateral and medial meniscus of the knee. BMJ Case Rep, 2017;bcr-2017-222232.
- Gunes T; Bostan B; Erdem M; Asci M; Sen C; Kelestemur MH. The “butterfly” suture technique for meniscal repair. Arch Orthop Trauma Surg, 2011; 131(3): 331–3.
- Guimaraes JB; Facchetti L; Schwaiger BJ; Gersing AS; Li X; Link TM. Natural evolution of popliteomeniscal fascicle tears over 2 years and its association with lateral articular knee cartilage degeneration in patients with traumatic anterior cruciate ligament tear. Eur Radiol, 2018; 28(8): 3542-9. DOI: 10.1007/s00330-017-5279-9.
- Stein G; Koebke J; Faymonville C; Dargel J; Müller LP; Schiffer G. The relationship between the medial collateral ligament and the medial meniscus: a topographical and biomechanical study. Surg Radiol Anat, 2011; 33(9): 763–66.
- Forkel P; von Deimling C; Lacheta L; Imhoff FB; Foehr P; Willinger L; et al. Repair of the lateral posterior meniscal root improves stability in an ACL-deficient knee. Knee Surg Sports Traumatol Arthrosc, 2018; 26(8): 2302-9. DOI: 10.1007/s00167-018-4949-8.
- LaPrade CM; James EW; Cram TR; Feagin JA; Engebretsen L; LaPrade RF. Meniscal root tears: a classification system based on tear morphology. Am J Sports Med, 2015; 43(2): 363–9.
- Natsis K; Paraskevas G; Anastasopoulos N; Papamitsou T; Sioga A. Meniscofibular ligament: morphology and functional significance of a relatively unknown anatomical structure. Anat Res Int, 2012; 2012: 214784.
- Onyema C; Oragui E; White J; Khan WS. Evidence-based practice in arthroscopic knee surgery. J Perioper Pract, 2011; 21(4): 128–34.
- Çetinkaya E; Kuyucu E; Gül M; Lapçin O; Albayrak K; Gürsu S. A suture technique for easier reduction and repair of bucket-handle meniscal tears while using the all-inside devices. SICOT-J, 2016; 2: 42.